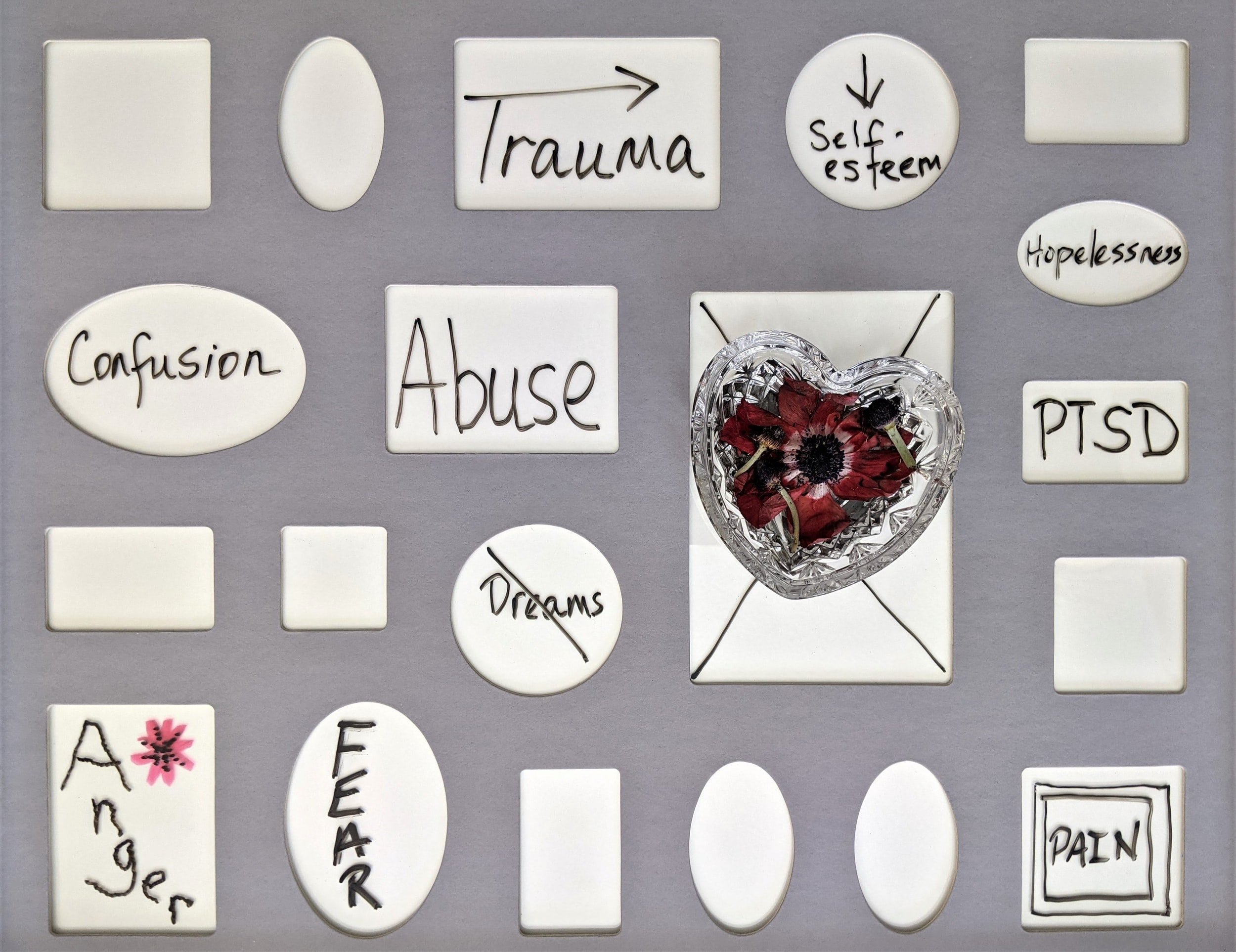
4 Veterans PTSD Myths and Truths That Every Civilian Needs To Know
If you think that veterans are characterized by PTSD (post-traumatic stress disorder) and physical wounds of war, then I’ve got news for you; veterans are much more than medals and scars.
In this Veterans Day post, I’m going to provide perspective about MYTHS & TRUTHS associated with veterans and PTSD. Not only will I discuss the most common myths regarding veterans and PTSD, but I’ll share some insight into truths.
“Veterans are much more than medals and scars.”
PTSD has been around since…
MYTH - Post-traumatic Stress Disorder has been an official diagnosis since the Vietnam War.
TRUTH - In the 1970s, post-traumatic stress disorder became a recognized grouping of psychological concerns for veterans returning home from war in Vietnam. PTSD became an operational diagnosis in 1980 with the publishing of the American Psychiatric Association’s third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III). Prior to this, the term “shell shock” was used to describe symptoms we now view as signs of PTSD. Shell shock was a term that was accredited to Charles Myers, an English Psychologist who first wrote about it in a 1915 publishing of The Lancet (he later admitted to not crafting the term himself). Initially, the symptoms of shell shock were contributed to the physical damages that affected soldiers that were exposed to bombardment in the trenches of World War I. It was within World War I that the term transitioned to describe a state of psychological concerns including debilitating anxiety, persistent nightmares, and physical afflictions ranging from diarrhea to loss of sight. These symptoms were appearing in soldiers who had never been directly under bombardment so the meaning of the term was broadened to include the psychological effects resulting from the experience of combat.
PTSD is only connected to combat
MYTH - Post-traumatic stress disorder is only experienced by those exposed to combat.
TRUTH - PTSD can result from exposure to death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence to include the following way(s)
Direct exposure
Witnessing the trauma
Learning of or indirect exposure to aversive details of the trauma, usually in the course of professional duties (medics, first responders)
People experience traumatic events that include circumstances such as car accidents, sexual assault, combat, workplace mishaps, and school violence. These events can be troubling for those who experienced it directly or vicariously.
PTSD vs. Complex-PTSD (C-PTSD)
MYTH - PTSD always leads to negative consequences in relationships and emotional dysregulation.
TRUTH - PTSD relates to a single traumatic episode. This can result in additional struggles due to increased worry and hyper-vigilance. C-PTSD relates to chronic or recurring exposure to threats or harm. Complex-PTSD (also known as complex trauma disorder) is distinct from PTSD since a distortion of a person’s core identity and emotional dysregulation can occur.
With PTSD, the main criterion include:
Sense of threat
Avoidance
Re-experiencing
With C-PTSD, the main criterion include:
Interpersonal disturbances
Negative self-concept
Affect dysregulation
Sense of threat
Avoidance
Re-experiencing
C-PTSD is commonly seen in:
Chronic sexual, psychological, or physical abuse
Intimate partner violence
Kidnapping & Human trafficking
Neglect
The way symptoms of PTSD and C-PTSD manifest is important to help distinguish the differences in each. PTSD is heavily guided by the post-traumatic symptoms to include nightmares, flashbacks, hyperarousal, startle response, paranoia, and burst of emotions. C-PTSD includes all of the aforementioned symptoms and changes in self-concept; how one sees themselves, their morals, and even their faith in others or their spirituality.
PTSD & Suicide
MYTH - PTSD leads to suicide since there is no hope. Suicidal people can’t cope and you can’t ask them if they might harm themselves.
TRUTH - PTSD can disrupt lives, but there is hope for a better tomorrow. PTSD alone doesn’t drive people to suicidal thoughts or actions, it is often an amalgamation of stressors - real or perceived - that may contribute to this state. This can include financial troubles, relationship difficulties, drug abuse, isolation, or loss of a friend/loved one. Suicide is something to be taken seriously and there is much work to be done to help those experiencing suicidal thoughts. Often times, simply listening to a person and providing them understanding (to the best of one’s ability) to encourage them to receive help. It is okay to ask if someone feels that they may harm themselves. It is okay to let them know you aren’t sure what to do but that you will do your best and also let them know that you might need help to better assist them. By supporting them embracing their healing through supportive treatment such as speaking with a professional, there is an increased chance for restoring hope in their lives. Take time to learn about resources that are available Nationally, Regionally, and Locally. Also know of services that are available 24/7 such as:
National Suicide Prevention Lifeline (confidential & free)
1-800-273-8255 (Option 1 for Veterans)
Lifeline Options For Deaf + Hard of Hearing
For TTY Users: Use your preferred relay service or dial 711 then 1-800-273-8255.
In conclusion, PTSD & veterans…
PTSD and C-PTSD can be experienced by anyone. Often, PTSD is made synonymous with veterans through societal narratives that usually reflect only one piece of the whole person. Celebrate veterans on Veterans Day and be an advocate for healing. Your kindness might comfort them now or in the future.